Causes of dementia
Dementia is a state of impaired health caused by various diseases. The most common causes are brain disorders where nerve cells gradually deteriorate due to neurodegenerative processes or are no longer adequately supplied with energy because of vascular changes in the brain.
Neurodegenerative diseases
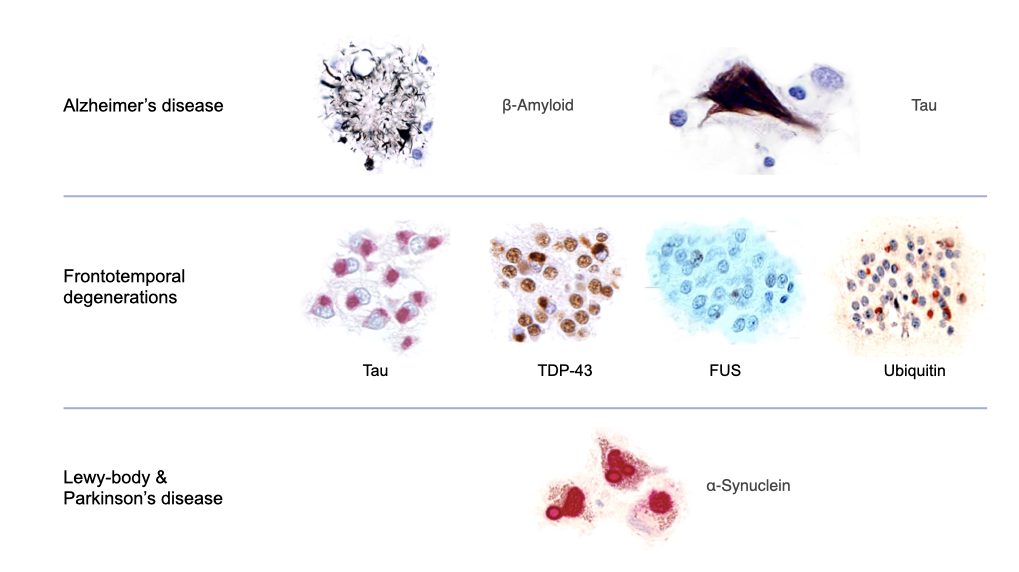
The most frequent causes of dementia are neurodegenerative diseases where nerve cells are gradually lost. Among the neurodegenerative diseases, Alzheimer’s disease is the most common, followed by frontotemporal degenerations, and Lewy body diseases (which include Parkinson’s disease). In the neurodegenerative diseases, errors in the processing of nerve cell proteins lead to the accumulation and deposition of the modified proteins within and outside of nerve cells, which has a negative impact on nerve cell functioning and viability.
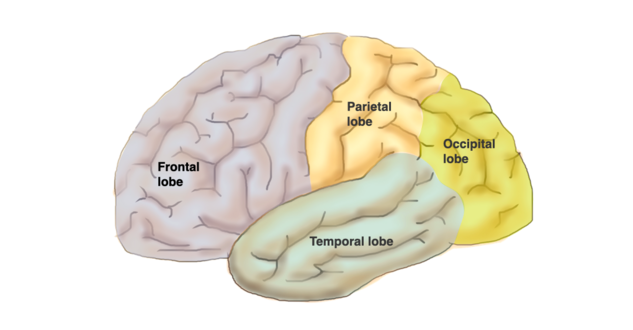
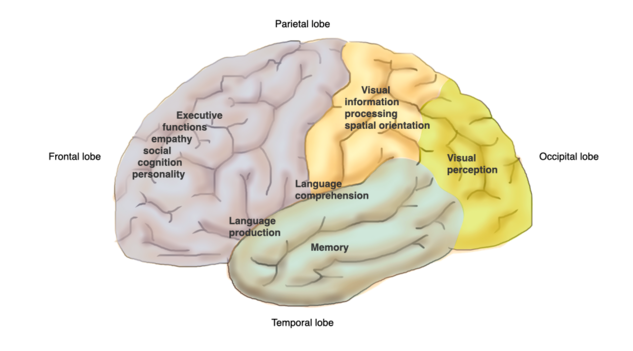
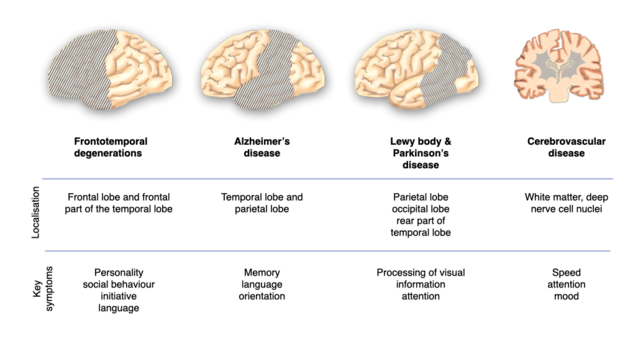
Alzheimer's disease is a brain disorder characterized by changes in two specific proteins. These alterations affect the function of nerve cells and lead to their demise. The temporal and parietal lobes of the brain are particularly affected.
The two proteins involved are β-amyloid, which accumulates outside nerve cells forming plaques, and tau, which accumulates inside nerve cells forming neurofibrillary tangles. Alzheimer's disease develops over many years, long before the first symptoms appear. It starts with the deposition of β-amyloid and later results in decreased brain activity, which can be visualised through positron emission tomography (PET) scans. This process leads to brain shrinkage, especially in the hippocampus, which can be detected using magnetic resonance imaging (MRI). Hippocampal shrinkage adversely affects memory.
Frontotemporal Degenerations:
Frontotemporal degenerations are various brain disorders. They differ in the symptoms they cause and how they affect the brain. What they have in common is that they only affect the front parts of the brain, such as the frontal lobe and the anterior part of the temporal lobe. The changes that occur in these diseases involve various proteins, one of which is called tau.
Lewy Body Disease:
In Lewy body diseases, including Parkinson's disease, round deposits called Lewy bodies form in nerve cells, especially in the back of the brain. These deposits consist of a normal cell protein called α-synuclein. The exact causes of these protein problems are not fully understood but could involve genetic factors and difficulties in clearing waste products from the brain.
The origins of these processes (e.g., genetic predisposition, defective clearance mechanisms) are only partly known.
Cerebrovascular diseases
The second most common cause of dementia is cerebrovascular diseases, which affect the small blood vessels in the brain. These blood vessels supply the brain with blood, oxygen, and nutrients. Deposits or blood clots in the vessel walls disrupt the energy supply to nerve cells and often occur in conjunction with Alzheimer's disease.
There are different forms of cerebrovascular dementia:
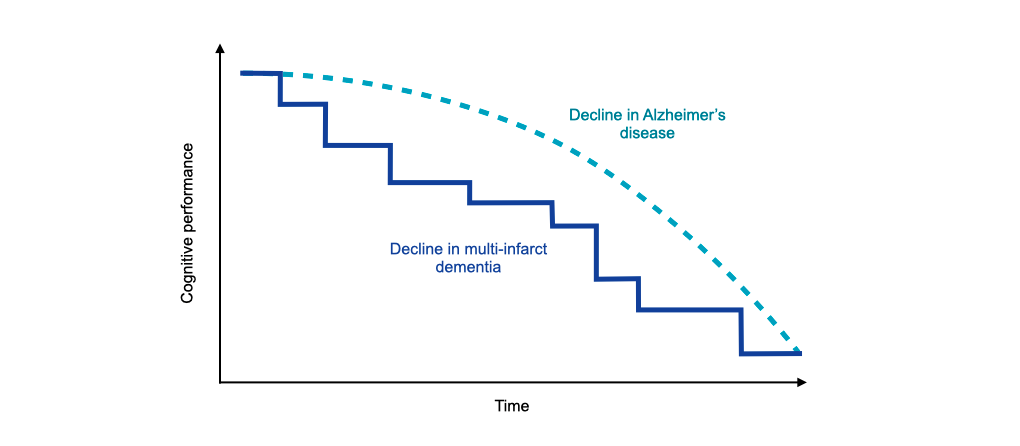
- Changes in small blood vessels in the brain that gradually impair cognitive function.
- Multiple small cerebral infarctions, which manifest as consecutive strokes and lead to "multi-infarct dementia," where cognitive abilities gradually decline.
- Single cerebral infarctions in critical areas that occur suddenly, similar to strokes.
- Brain hemorrhages or chronic circulation problems, often due to narrowing of the neck vessels
Potentially reversible causes of dementia
Only rarely (less than 2%) can dementia be treated. Treatable causes include:
Normal pressure hydrocephalus: Accumulation of fluid in the brain, leading to symptoms such as urinary incontinence, gait disturbances, and dementia.
Underactive thyroid or overactive parathyroid: Imbalances in thyroid hormones can cause memory impairments and other symptoms.
Excessive alcohol abuse: Chronic alcohol consumption can damage the brain and increase the risk of dementia.
Vitamin deficiency: Lack of Vitamin B12 or folic acid can lead to anemia, nerve damage, and cognitive impairments.
Depression: Depression is a risk factor for dementia, possibly due to changes in brain vessels and stress hormones.
Detecting and treating the underlying cause can improve or even reverse dementia symptoms.
Localisation determines the clinical picture
The different parts of the brain have different functions. Therefore, the symptoms of dementia depend on the location of the underlying brain disease. The location in a certain part of the brain leads to a specific clinical picture of dementia.
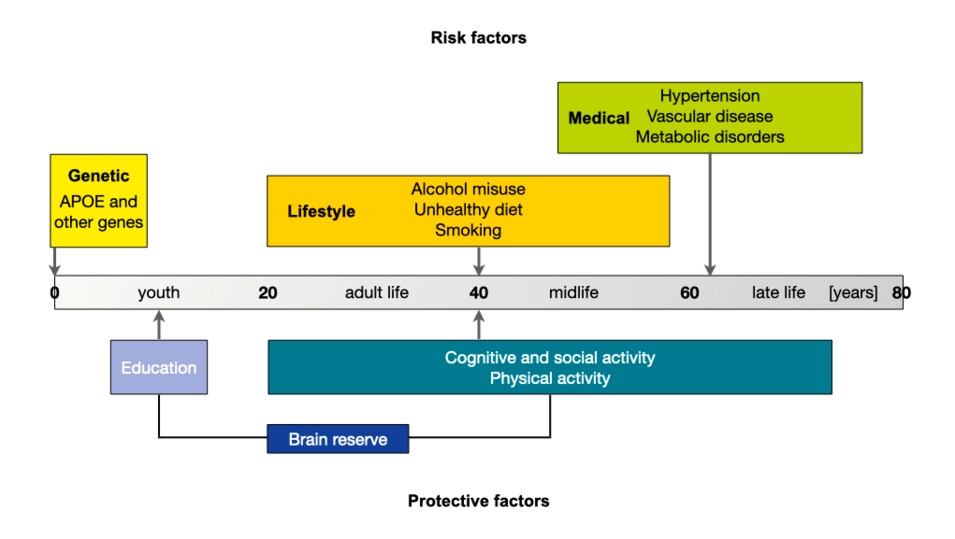
Risk factors for developing diseases causing dementia
The likelihood of developing dementia is influenced by many factors. Some of these factors are non-modifiable, such as age and genetic risk factors. These genetic factors include very rare mutations in specific genes with a strong effect (the mutation triggers the disease) and common variants of genes with a weaker effect (the variant simply increases the likelihood of the disease occurring). About a quarter of the population has at least one case of dementia known in the family. In these families, the risk for family members to develop dementia is approximately twice as high (20%) as the population average (10%).
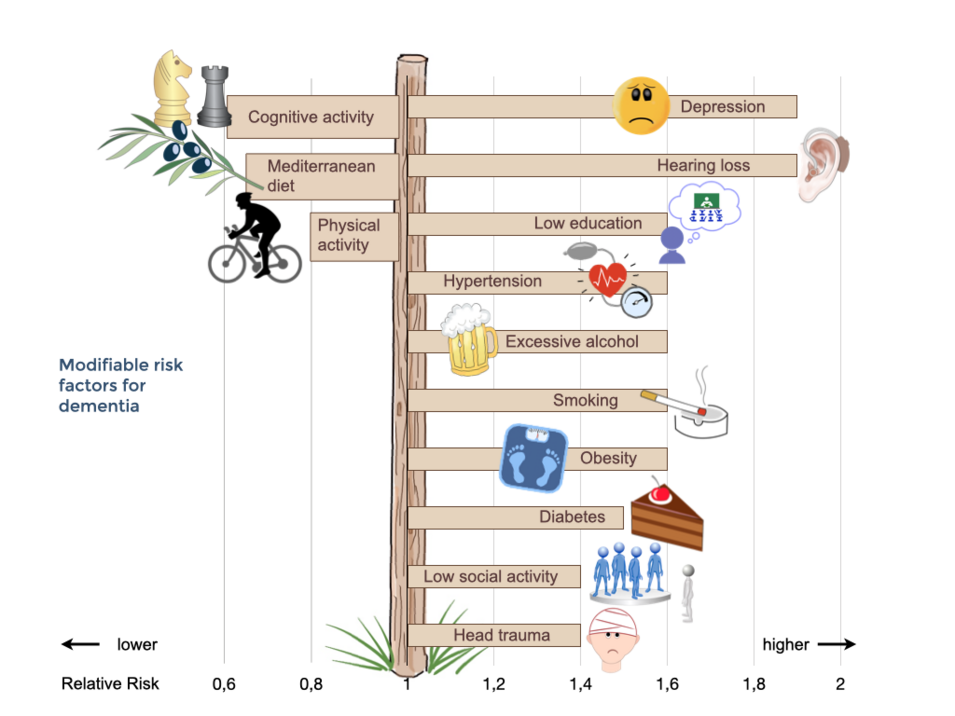
Fortunately, many risk factors for dementia are modifiable. These include medical factors such as diabetes, high blood pressure, obesity, and depression, as well as lifestyle factors such as lack of physical activity, smoking, and low educational level. Additionally, there are protective factors such as physical and mental activity that reduce the risk of dementia.
Co-morbid conditions
As most people with dementia belong to an older age group, they are more likely to have multiple, often chronic, health problems in addition to dementia. These need to be treated appropriately to minimize cognitive and everyday limitations, avoid or mitigate behavioral changes, and maintain a satisfactory quality of life. Dementia can complicate the treatment of these co-morbidities and limit a person's ability to cope with health problems.
Some physical problems are more common in people with dementia than in adults of the same age without cognitive impairment. These include falls, delirium (acute states of confusion), epileptic seizures, weight loss, malnutrition, type 2 diabetes, incontinence, sleep problems, dental problems, impaired sexual function, and frailty. Around 25% of people with dementia suffer from depression that requires treatment.
References
- Bateman RJ, Xiong C, Benzinger TLS, et al. Clinical and biomarker changes in dominantly Inherited Alzheimer’s disease. N Engl J Med 367: 795-804, 2012
- Beyer K, Domingo-Sàbat M, Ariza A. Molecular pathology of Lewy Body diseases. Int J Mol Sci 10:724-745, 2009
- Byers AL, Yaffe K. Depression and risk of developing dementia. Nat Rev Neurol 7: 323-331, 2011
- Bunn F, Burn A-M, Goodman C, et al. Comorbidity and dementia: a scoping review of the literature. BMC Medicine 12: 192, 2014
- Cairns NJ, Bigio EH, Mackenzie IRA, et al. Neuropathologic, diagnostic and nosologic criteria for frontotemporal lobar degeneration: consensus of the Consortium for Frontotemporal Lobar Degeneration. Acta Neuropathol. 114: 5-22, 2007
- Damasceno BP. Neuroimaging in normal pressure hydrocephalus. Dement Neuropsychol 9: 350-355, 2015
- Dugbartey AT. Neurocognitive aspects of hypothyroidism. Arch Intern Med 158: 1413-1418, 1998
- Goebels N, Soyka M. Dementia associated with vitamin B12 deficiency. J Neuropsychiatry 12: 389-394, 2000.
- Jack CR, Knopman DS, Jagust WJ, et al. Tracking pathophysiological processes in Alzheimer’s disease: an updated hypothetical model of dynamic biomarkers. Lancet Neurol 12 :207-216, 2013
- Kivipelto M, Solomon A, Ahtiluoto S, et al. The Finnish Geriatric Intervention Study to Prevent Cognitive Impairment and Disability (FINGER): Study design and progress. Alzheimers Dement 9: 657-665, 2013
- Kuring JK, Mathias JL, Ward L. Prevalence of depression, anxiety and PTSD in people with dementia: a systematic review and meta-analysis. Neuropsychol Rev 28: 393-416, 2018
- Little MO. Reversible dementias. Clin Geriatr Med 34:537-562, 2018
- Mackenzie IRA, Rademakers R. The molecular genetics and neuropathology of frontotemporal lobar degeneration: recent developments. Neurogenetics 8: 237-248, 2007
- Norton S, Mathews FE, Barnes DE et al. Potential for primary prevention of Alzheimer’s disease: an analysis of population-based data. Lancet Neurol 13: 788-794, 2014
- Reynolds EH. Folic acid, ageing, depression, and dementia. BMJ 324: 1512-1515, 2002
- Warren JD, Rohrer JD, Rossor MN. Frontotemporal dementia. BMJ 347: f4827, 2013
- Wiegmann C, Mick I, Brandla EJ, Heinz A et al. (2020). Alcohol and dementia – what is the link? A systematic review. Neuropsychiatr Dis Treat 16: 87-99, 2020